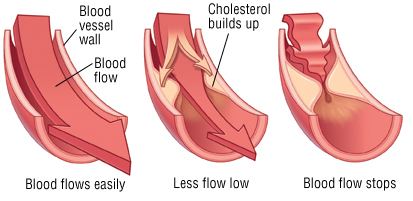
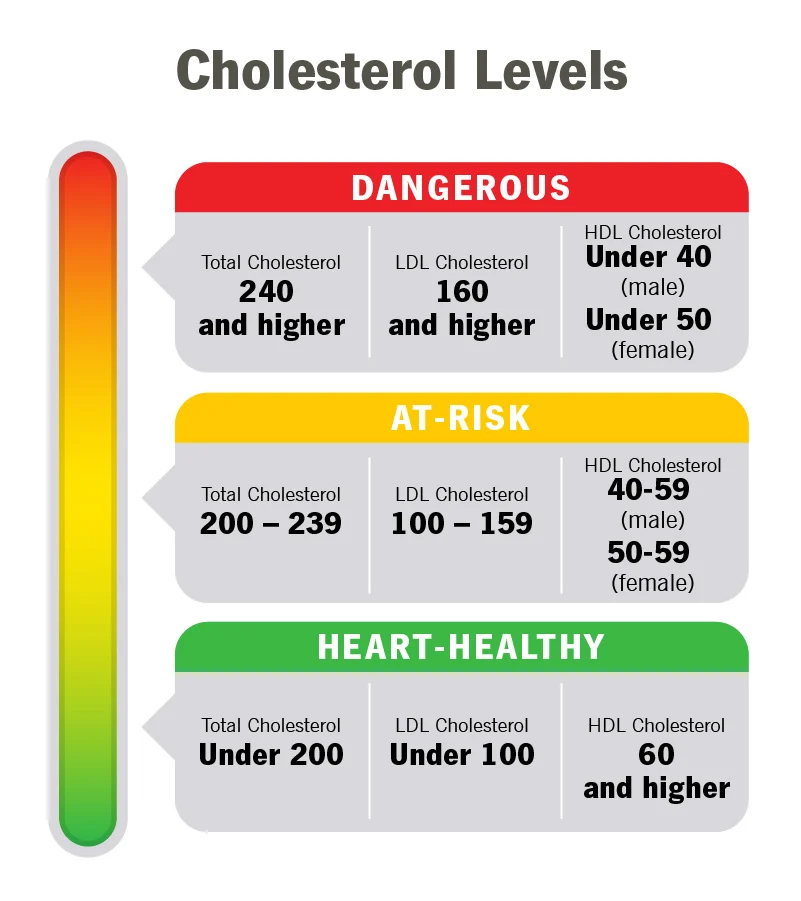
Hypercholesterolemia is the diagnosis of having elevated levels of cholesterol in the blood. It is a type of hyperlipidemia (high levels of lipids in the blood). Cholesterol is measured through blood analysis, and can be affected by diet so much that a fasting blood sample is necessary to gain accurate results. Cholesterol is a naturally occurring substance in the body that is necessary for cell growth. It is when patients have too much cholesterol or problems with cholesterol regulation in the body that high levels can become problematic. While the word lipid is often considered a synonym for fats, fats are actually a type of lipid called triglycerides. The body needs cholesterol, fats, lipids and triglycerides, however when there is an overabundance or improper regulation occurs, patients may experience problems.
Lipid disorders, also called dyslipidemias, are abnormalities of lipoprotein metabolism and include elevations of total cholesterol, Low Density Lipoprotein (LDL) cholesterol, or triglycerides; or deficiencies of HDL (High Density Lipoprotein) cholesterol. These disorders can be acquired or familial (for example, familial hypercholesterolemia). Total cholesterol is a generic overall value, while HDL is a healthy form of cholesterol and LDL is a bad form of cholesterol. LDL can further be analyzed for variations in fluffy sticky cholesterol cells as opposed to smaller and less serious cells. To remember the difference between HDL and LDL, just remember that “H” stands for healthy.
Understanding Lab Values:
- Total blood cholesterol: This includes your HDL, LDL, and 20 percent of your total triglycerides.
- Triglycerides: This number should be below 150 mg/dL. Triglycerides are a common type of fat. If your triglycerides are high and your LDL is also high or your HDL is low, you’re at risk of developing atherosclerosis.
- HDL: The higher this number, the better. It should be at least higher than 55 mg/dL for females and 45 mg/dL for males. HDL is “good cholesterol.”
- LDL: The lower this number, the better. It should be no more than 130 mg/dL if you don’t have heart disease, blood vessel disease, or diabetes. It should be no more than 100 mg/dL if you have any of those conditions or high total cholesterol.
What you can do:
- Decrease fat intake: The total fat in your diet should be cut back to no more than 30% of your daily caloric intake. For instance, if you consume 1,800 calories per day, you should get no more than 600 calories from fat. Reduce fatty foods such as meats, dairy (dairy milk & cheeses), egg yolks, and oils like coconut and palm. You can substitute for lower fat options like using cooking oil sprays, margarine, or canola oil. Avoid trans fats. Learn more about Trans Fats here: https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/trans-fat
- Reduce meat intake: Pork, lamb, and beef are higher in fat than chicken and fish. Choosing leaner cuts such as eye of round and pork tenderloin can help too. Trim fatty portions from meats if you are cooking at home. Choose smaller portions- 3 ounces of meat is plenty. You can choose other foods like beans, and vegetables and protein substitutes.
- Increase fiber intake: Fiber can reduce risk of heart disease. Foods high in fiber include nuts, seeds, legumes (peas, lentils, edamame, black beans, and kidney beans), whole grains (barley, oats – oatmeal is a great addition to a cholesterol lowering diet- whole wheat breads and whole wheat pastas), vegetables, and fruits (especially blackberries, grapefruits, apples, bananas, pears, and oranges).
- Lower alcohol intake: Too much alcohol can boost triglycerides. Excess alcohol is linked to obesity and weight gain. “Moderate alcohol use” means no more than 2 drinks per day for men and no more than 1 drink per day for women. Avoiding alcohol altogether is even better.
- Exercise regularly: A minimum of 2.5 hours of exercise per week is recommended to include running, swimming, walking, weight lifting, yoga, and hiking. Slowly increase your time by starting out with 10-15 minutes and gradually increase your time to ease into a more regular schedule.
References:
https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
https://www.heart.org/en/health-topics/cholesterol
Brian holds a Master degree in Health Administration (MHA), a Bachelor of Science in Health Sciences (BSHS), and a Certificate in Clinical Bioethics which bestows the ability to serve on ethics boards, help make healthcare decisions, and provide continuing medical education.
He is a national author and speaker and health consultant in all aspects of healthcare delivery, with special interests in risk adjustment, population health, public health, clinical bioethics, patient safety, and patient education.
*All posts and materials posted here are for education and demonstration purposes and are not intended to be medical advice. It is important to remember that every person is unique with unique diagnoses, and may be taking different prescriptions and supplements. I encourage each person to discuss your conditions with a trusted healthcare provider and be engaged to learn along your individual path to wellness.