The heart is a uniquely special and important organ. Medical issues that can occur with the heart can involve many areas to include blockages of the vessels, issues with the fitness of the muscular tissues of the heart, infections of the heart, valve issues, and various rhythm issues which are commonly known as cardiac conduction disorders. These rhythm issues are presented below.
Cardiac Conduction Disorders
Common cardiac conduction disorders include supraventricular tachycardia, AV blocks, sick sinus syndrome, atrial/ventricular fibrillation, and atrial/ventricular flutter.
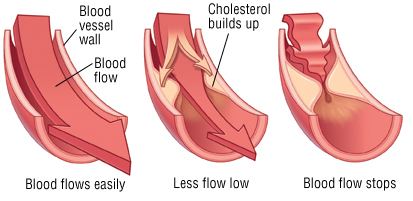
It is helpful to have a basic understanding of how the heart’s electrical system works before discussing the various conduction disorders that can occur. The heart is a muscle, which also has its own electrical system. Many may be more familiar with cardiac problems that can occur due to arterial clogging or blockages, such as coronary artery disease (CAD), or there may be a disease complication affecting the muscle of the heart causing it to become weak, such as in cardiomyopathy. When the electrical impulses have problems or difficulties, a cardiac conduction disorder may occur. There are many different types of cardiac conduction disorders and some patients can experience these intermittently, while others may persist for a chronic period of time or may be life-long. Some patients have more than one conduction disorder simultaneously. Possible treatments for conduction disorders include surgery, ongoing medication and observation, or an electrical assistive device implant.
The Sino Atrial (SA) node, located in the upper right quadrant of the heart, is the pacemaker of the heart. The SA node sends an electric signal that prompts the heart to contract/pump. When this signal is blocked, interrupted, sent too frequently or infrequently, or the ventricular response is out of sync, conduction disorders may occur. Conduction disorders can develop over time, can be caused by medications, consuming other supplements, foods, or drinks, or can be congenital.
Think of the heart as a square with upper and lower portions. Example:
Chambers of Heart Example
Right Atrium | Left Atrium |
Right Ventricle | Left Ventricle |
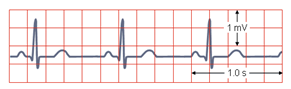
Measure of Heart Rate Example
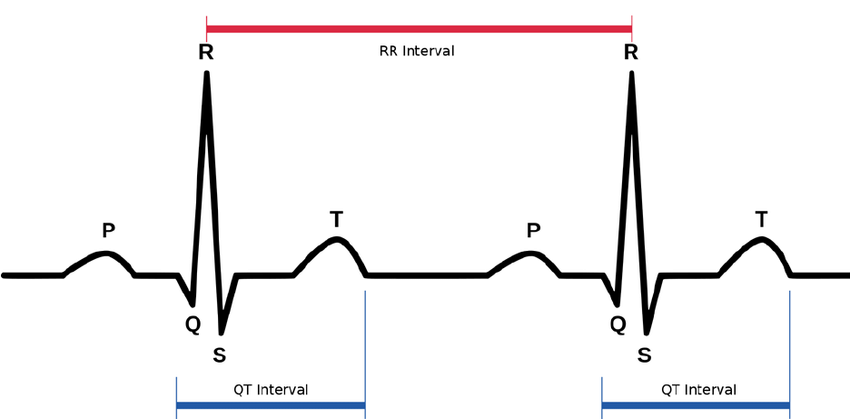
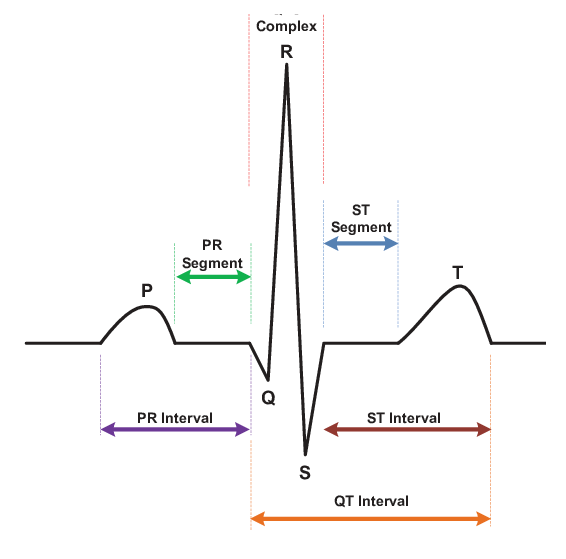
In the diagram above of a normal heartbeat, the “P” is the SA node’s (Right Atrium) electrical impulse for the heart to pump or beat, the QRS is the ventricular (Right & Left Ventricles) response (heartbeat), and the “T” is a re-polarization of electrical energy for the process to repeat itself. These points are measured when reviewing various heart conduction disorders and help identify where the conduction disorders may be occurring.
Various intervals between complexes are measured to analyze heart rhythms.
Figure: Heartbeat Dissected
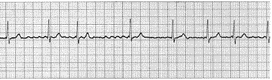
In a NSR (Normal Sinus Rhythm), all complexes are normal, evenly spaced, with a rate of 60-100 beats per minute.
Example of Normal Sinus Rhythm
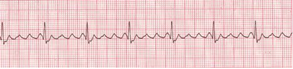
Bradycardia is a slower than normal heart rate. Tachycardia is a faster than normal heart rate. Both are a normal part of daily heart function and response.
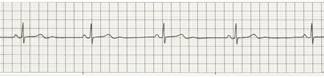
Example of a Sinus (normal) Bradycardia
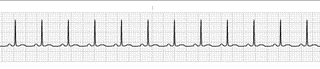
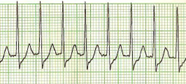
Example of a Sinus (normal) Tachycardia
An extremely slow or persistently-below-normal heart rate often is due to a malfunctioning SA node. The condition is called sick sinus syndrome. The typical intervention for a sick sinus syndrome is the placement of a pacemaker to make the heart rate normal again. Various pacemaker models may be used.
Everyone’s heart rhythms vary, based on physical and emotional status, nutrition, and temperature. Each person’s pulse, or heart rate, can change from minute to minute. Likewise, heart rate will speed up (tachycardia) or slow down (bradycardia) as a response to physical and emotional factors. Cardiac conduction disorders can occur when these heart rates go too far beyond normal parameters (whether too fast or too slow). Many people will have skipped beats and bouts of fast and slow heart rates as a part of everyday life experiences. Only when these conduction disorders persist, create symptoms that would cause a concern for compounded problems, or are not addressed do they become a problem.
When a faster than normal heart rate originates at or above the atrioventricular node (AV), the condition is supraventricular tachycardia (SVT). Atrial fibrillation is a type of supra ventricular arrhythmia. In A-Fib (atrial fibrillation), there are irregular impulses reaching the AV node and only some are being transmitted. Another type of SVT is documented as paroxysmal supraventricular tachycardia (PSVT). The word paroxysmal means that there is a sudden burst or display of the tachycardia in portions or waves where there is a great intensity, which calms and then bursts forth in display again. A supraventricular tachycardia is a rapid atrial rhythm, while a ventricular tachycardia is a rapid ventricular rhythm.
Example of a Supraventricular Tachycardia (SVT)
Atrial Fibrillation/Flutter
Atrial Fibrillation
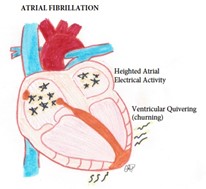
Example of Atrial Fibrillation
In the above examples, a clear difference between a normal heart rhythm and atrial fibrillation is clearly demonstrated. The placement of the P, QRS, and T waves are obviously out of rhythm. This is from the intense “shaking” or “churning” of the ventricles from the atrial hyperactivity or rapid firing of impulses. Atrial fibrillation is a very common diagnosis that is usually managed through blood thinning medications (such as Coumadin or warfarin) to prevent clots from forming from the churning activity. Sometimes atrial fibrillation can be a short event or converted and other times it is a life-long diagnosis. In some cases, a pacemaker may be implanted for the treatment of A-Fib, and if the patient has more than one conduction disorder, for example a history of sick sinus syndrome (or SA node malfunction) as well as A-Fib, and there is a pacemaker in place, the patient likely still has A-Fib and this can be revealed by the current use of Coumadin or warfarin, other blood thinner, or A-Fib medication. Pacemakers are most often implanted for SA node malfunction or sick sinus syndrome and not for A-Fib.
Example of Atrial Flutter
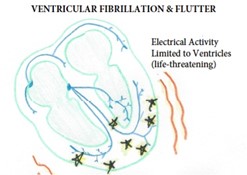
Ventricular Fibrillation (V-Fib)/Flutter (V-Flutter)
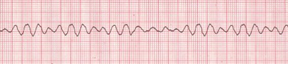
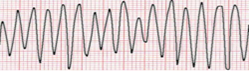
Ventricular fibrillation is a condition in which there is uncoordinated contraction of the cardiac muscle of the ventricles in the heart, making them “quiver” rather than contract properly. It is life threatening and requires immediate attention for life-saving purposes. Ventricular flutter is an arrhythmia, more specifically a tachycardia that affects the ventricles with a rate of over 200 beats per minute. It has been considered as a transition between ventricular tachycardia and fibrillation. It is a critically unstable arrhythmia that can result in sudden cardiac death. Both of these conduction disorders require cardioversion (shock treatment) as well as medication support. Patients who have had known problems with short runs of these arrhythmia’s may be placed on an Automatic Internal Cardiac Defibrillator (AICD) which is a special pacemaker than can monitor for problem rhythms and shock the patient when necessary.
Ventricular Fibrillation/Flutter
Example of Ventricular Fibrillation
Example of Ventricular Flutter
Atrioventricular (AV) Block
When the SA node sends its electrical impulse downward through the heart, the electrical impulse runs along a normal pathway. These bundles (or electrical lines) can become blocked for various reasons, causing a “bundle branch block.” When this occurs, something is blocking the normal flow of the signal, which results in a form of AV block. There is a disruption of the electrical message between the atrium (top of the heart) and the ventricles (bottom of the heart).
Documentation of AV blocks is important because there are many different types of blocks. The blocks are classified by measurements of the PR interval in the heartbeats (mentioned earlier) and are often named for physicians who discovered them.
Electrical System of Heart
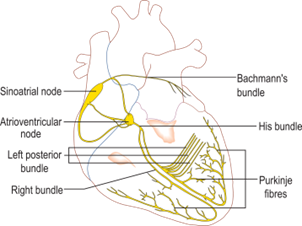
- First Degree AV Block: PR interval is greater than 0.20 sec.
- Second Degree AV Block:
- Type I (also known as: Mobitz I, or Wenkebach): Progressive prolongation of PR interval with dropped beats (the PR interval gets longer and longer, and finally one beat drops).
- Type II (also known as: Mobitz II, or Hay): PR interval remains unchanged prior to the P wave, which suddenly fails to conduct to the ventricles.
- Third Degree AV Block (Complete): No association between P waves and QRS complexes.
Bundle Branch Block: General defects in the electrical conduction system of the heart between the atrial and ventricle portions of the heart. Bundle branch blocks are fairly common and often do not cause any issues.
Heart conduction disorders can be serious. some patients might discount dizziness or fatigue to the causes of their symptoms, and older patients may experience age prejudice related to potential dementia or simple aging when a cardiac condition may be underlying. It is important to discuss all symptoms in detail with your healthcare provider so that the appropriate tests can be performed.
Diagnostic testing can include blood work, cardiac monitoring, exercise stress testing, and echocardiograms. Such testing is chosen based on the symptoms being presented in an effort to discover what issues might be present and which treatments might be best for each patient.
Brian holds a Master degree in Health Administration (MHA), a Bachelor of Science in Health Sciences (BSHS), and a Certificate in Clinical Bioethics which bestows the ability to serve on ethics boards, help make healthcare decisions, and provide continuing medical education.
He is a national author and speaker and health consultant in all aspects of healthcare delivery, with special interests in risk adjustment, population health, public health, clinical bioethics, patient safety, and patient education.
*All posts and materials posted here are for education and demonstration purposes and are not intended to be medical advice. It is important to remember that every person is unique with unique diagnoses, and may be taking different prescriptions and supplements. I encourage each person to discuss your conditions with a trusted healthcare provider and be engaged to learn along your individual path to wellness.